How can MEDOMENT Optimise Patient Engagement?
October 14, 2022
Can Telemedicine Improve Diabetes Management?
January 8, 2023Telemedicine is improving healthcare delivery by expanding access, enhancing patient engagement and increasing collaboration between patients and healthcare providers. When used appropriately alongside in-person care, telemedicine can help to improve outcomes while providing time and cost-efficiencies.
Although there are challenges associated with providing care through a screen, there are ways to adapt consultations. In many cases, it is possible to conduct a physical examination virtually with the right equipment and cooperation of the patient.

When can a physical examination be done virtually?
The key to the effective use of telemedicine is using professional judgement to decide when you need to bring your patient into the clinic for a consultation, tests or treatment. A video consultation can be used to triage patients who may need in-person care. Telemedicine is ideally suited to non-emergency, chronic or stable conditions. Serious and high-risk cases should be seen in person.
Many physical signs and symptoms can be assessed remotely. Patients must be able to give informed consent for teleconsultation. With good instructions, a physician-directed self examination can be performed for many conditions, with or without the help of a family member or carer. However, internal examinations, high-tech diagnostic imaging or lab tests will require an in-person visit.
Set up for a virtual physical examination
See this blog article for a step-by-step guide to teleconsultations. Here, we will concentrate on aspects related to virtual physical examinations.
Device and technical considerations
● Mobile, handheld devices are preferable, as you can ask the patient to move the camera around for better visibility. Many also have a flashlight and the ability to zoom the image in or out.
● Good lighting is essential. If possible, ask the patient to sit in a room with natural light from a large window. Otherwise, a good lamp with a white bulb can be used.
● Find out what home equipment can be made available such as a thermometer, weighing scale, blood pressure monitor, or glucometer for diabetics.
● Ensure that both sides of the call have a reliable internet connection.
● Check your telemedicine platform complies with the relevant data protection regulations, such as HIPAA.

During the teleconsultation
Observe the patient’s physical appearance, breathing, level of alertness and fluency of speech etc. As with an in-person visit, obtaining a thorough account of the patient’s presenting complaint and medical history is crucial. Listen carefully and relay back what you have heard to confirm and correct any misunderstandings. This will help you decide how to direct the examination.

Conducting a virtual physical examination
Clearly explain and demonstrate to the patient, and relative or carer if present, what you want them to do. Document your observations including what was done by the patient and what was unable to be performed and the reason, such as lack of at-home equipment.

Assessing vital signs
- Body temperature – instruct correct use of home thermometer.
- Pulse/heart rate – show the patient how to find their pulse on their wrist, ask them to count beats aloud while you time 15 seconds then multiply by 4. (Heart rate can be measured with a digital BP monitor.)
- Respiration rate – Observe breathing rate over 15 seconds and multiply by 4.
- Blood pressure – Instruct correct use of home BP monitor.
- BMI – ask the patient (or their carer) to measure height in cm and weight in kg. BMI = weight in kg/(height in cm)2. If not practical, record your impression of the patient’s constitution.

System specific examination
Ears/Nose/Throat/Eyes – Ask the patient to move the camera closer to the relevant body part. Request additional light source to be used as required. Ask the patient to percuss over the sinus areas for tenderness.
Skin – Assess for rashes, jaundice, flushing or pallor. Ask the patient to self-describe the rash and press to observe for blanching.
Respiratory – Ask the patient to take a deep breath in and out. Listen for wheezing or coughing and assess inspiratory/expiratory ratio. Instruct patients on use of a peak flow meter.
Cardiovascular – Ask the patient to press on lower extremities to check for oedema.
View the neck to look for distension of jugular veins. Evaluate skin for ecchymosis or telangiectasia.
Lymphatic – Show the patient how to feel for lymph nodes and self-palpate for cervical or axillary lymphadenopathy.
Musculoskeletal – Instruct the patient to perform exercises to assess range of motion. Visualise joints to look for erythema and ask the patient to assess warmth, tenderness or pain. Assess gait.
Gastrointestinal/abdominal – Show a family member or carer how to do soft and deep abdominal palpation in different quadrants, or ask the patient to self-palpate. Patients can describe and point to the location of symptoms such as pain.
Diabetes – Instruct patients on the use of a home glucometer to measure blood sugar.
Neurological – Request the help of a relative or carer to test for strength and sensation and assess symmetry. Show how to use a flashlight to test pupillary reaction. Give instructions to follow a finger to observe for ocular movements. Ask the patient to fully extend arm then touch their nose. Assess facial movements.

New wearable technologies and digital tools
More advanced digital tools are starting to become available such as at-home digital stethoscopes, otoscopes and single-lead ECG. Wearable technology is also rapidly advancing. Patients may already have smart watches with the ability to measure their pulse and blood oxygen level.
At the end of the consultation
Ensure that the visit is correctly documented for medical records and insurance purposes. Screenshots of relevant findings, taken with the patient’s consent should be securely stored. Summarise the consultation, check if the patient has understood
the discussion and ask if they have any questions. Decide on the need for referral or follow-up and whether this should be virtual or in-person.
Are you looking for the ideal telemedicine software?
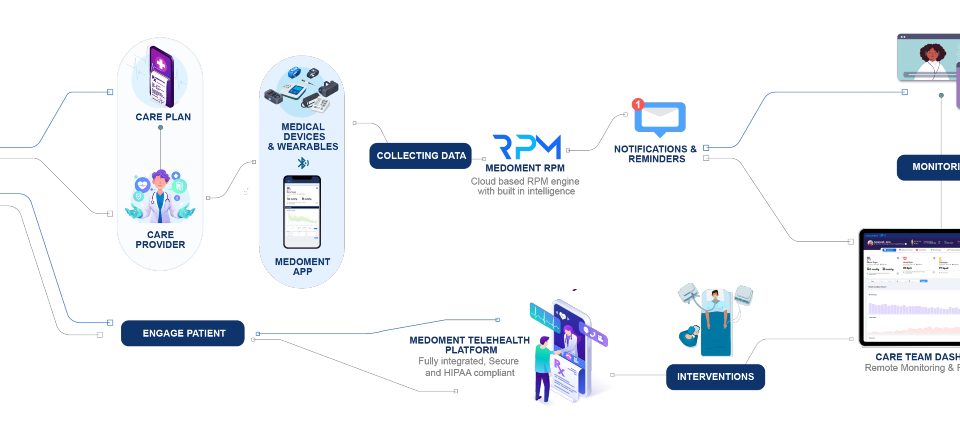
Medoment is the comprehensive solution for the management of both in-person and virtual medical care. Designed by the experts in healthcare informatics at HT Works, Medoment offers online consultation scheduling, teleconsultations, an innovative patient engagement portal and more, within a single platform.
To find out more, or book a demonstration, contact us today:
Dubai: +971 50 235 4021
London: +44 208 049 9549
Colombo: +94 77 700 6080
info@medoment.com
RECENT POSTS
- 7 Benefits of Medoment RPM for Your Practice
- Remote Patient Monitoring for Chronic Disease Management
- Can telemedicine help reduce the impact of cardiovascular diseases?
- Can telemedicine be used during pregnancy?
- Can Telemedicine Improve Diabetes Management?
- How to conduct a physical exam via telemedicine
- How can MEDOMENT Optimise Patient Engagement?
- Can patient engagement portals improve healthcare?
- How to choose the right telemedicine software partner
- How to invest in telemedicine software